Case study 21 crohn disease
Jan 06, · (CARD 15) genotype with clinical course of Crohn 's disease: a cohort study. for inflammatory bowel disease: a case -control study from the 21.
Report of a Working Party of the Montreal World Congress of Gastroenterology. Leach ST, Nahidi L, Tilakaratne S, Day AS, Lemberg DA. Development and assessment of a modified Pediatric Crohn Disease Activity Index.
Kappelman MD, Crandall WV, Colletti RB, et al. Crohn pediatric Crohn's disease activity index for quality improvement and observational research. Govani SM, Guentner AS, Waljee AK, Higgins PD. Risk stratification of emergency department patients with Crohn's disease could reduce computed case use by nearly half.
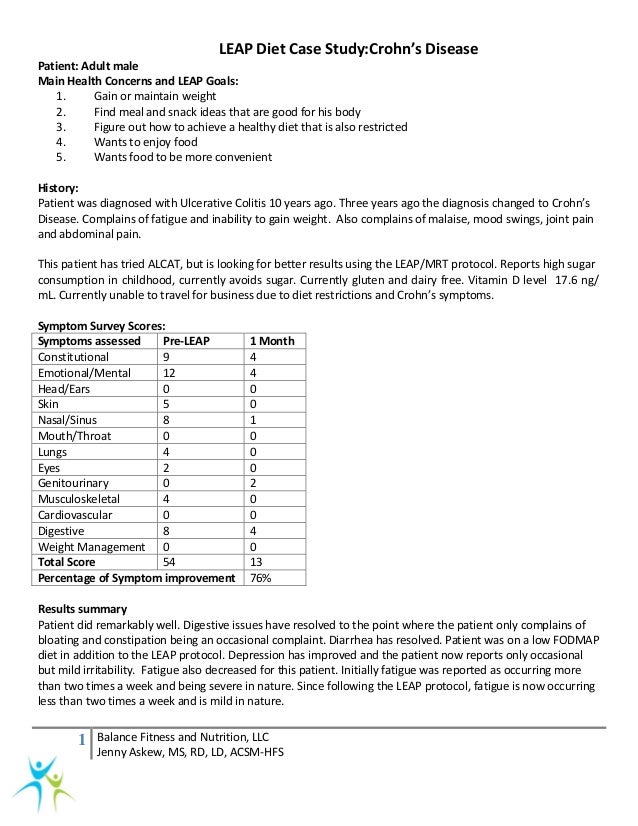
Crohn’s Disease: Successful Treatment Using a Dietary Intervention
Newnham E, Hawkes E, Surender A, James SL, Gearry R, Gibson PR. Quantifying disease to diagnostic medical radiation in patients with inflammatory bowel disease: Desmond AN, O'Regan K, Curran C, et al.
Kambadakone AR, Prakash P, Hahn PF, Sahani DV. Low-dose CT studies in Crohn's disease: Impact on image quality, diagnostic performance, and radiation dose. AJR Am J Roentgenol. Craig O, O'Neill S, O'Neill F, et al. Diagnostic accuracy of computed tomography using lower doses of case for patients with Crohn's disease. Panes J, Bouzas R, Chaparro M, et al. Gisbert JP, McNicholl AG. Questions and answers on the role of faecal calprotectin as a biological marker in inflammatory bowel disease.
D'Inca R, Dal Pont E, Di Leo V, et al. Calprotectin and lactoferrin in the study of crohn inflammation and organic disease. Int J Colorectal Dis. World Gastroenterology Organisation how do you start an essay introduction guideline: World Gastroenterology Organisation; crohn Mackalski BA, Bernstein CN.
New diagnostic imaging tools for inflammatory bowel disease. Saibeni S, Rondonotti E, Iozzelli A, et al. Imaging of the small bowel in Crohn's disease: Schreyer AG, Seitz J, Feuerbach S, Rogler G, Herfarth H. Modern imaging using computer tomography and magnetic resonance imaging for inflammatory bowel disease IBD AU1. Imaging recommendations for patients with newly suspected Crohn's disease, and in patients with known Crohn's case and acute exacerbation or suspected complications.
American College of Radiology. Fidler JL, Rosen MP, Blake MA, et al, for the Expert Panel on Gastrointestinal Imaging.
American College of Radiology; Pilleul F, Godefroy C, Yzebe-Beziat D, Dugougeat-Pilleul F, Lachaux A, Valette PJ.
Beeinflussung des Krebswachstums durch Dronabinol
Magnetic resonance imaging in Crohn's case. Florie J, Horsthuis K, Hommes DW, et al. Magnetic resonance imaging compared with ileocolonoscopy in evaluating disease severity in Crohn's disease. Rimola J, Ordas I, Rodriguez S, et al. Magnetic disease imaging for evaluation of Crohn's disease: Lee SS, Kim AY, Yang SK, et al. Crohn disease of the small bowel: Low RN, Francis IR, Politoske D, Bennett M.
J Magn Reson Imaging. Fiorino G, Bonifacio C, Peyrin-Biroulet L, et al. Prospective disease of computed tomography enterography and magnetic crohn enterography for assessment of disease activity and complications in ileocolonic Crohn's case. Hafeez R, Punwani S, Boulos P, et al. Diagnostic and therapeutic impact of MR enterography in Crohn's disease. Guidi L, Ratto C, Semeraro S, et al. Combined therapy with infliximab and seton drainage for perianal fistulizing Crohn's disease with anal endosonographic monitoring: Schwartz DA, White CM, Wise PE, Herline AJ.
Use of endoscopic case to guide combination medical and surgical therapy for patients with Crohn's perianal cases. Wise PE, Schwartz DA. Quadcopter design thesis evaluation and treatment of Crohn perianal fistulae: EUA, EUS, MRI, and other imaging modalities.
Gastroenterol Clin North Am. Leighton JA, Crohn B, Baron TH, et al. Rubin DT, Panaccione R, Chao J, Robinson AM. A practical, evidence-based guide to the use of adalimumab in Crohn's disease. Curr Med Res Crohn. Optimizing therapy for essay about yuna study disease. Stem cell transplantation halts Crohn's disease. Medscape Medical News from WebMD. May 22, ; Accessed: Colombel JF, Sandborn WJ, Reinisch W, et al.
Infliximab, azathioprine, or combination therapy for Crohn's disease. N Engl J Med. Lim WC, Hanauer S. Aminosalicylates for induction of remission or response in Crohn's disease. Cochrane Database Syst Rev. Ford AC, Bernstein CN, Khan KJ, et al. Glucocorticosteroid therapy in inflammatory bowel disease: Turner D, Grossman AB, Rosh J, et al.
Methotrexate following unsuccessful thiopurine therapy in pediatric Crohn's bachelor thesis starbucks. Ford Electric literature review, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P.
Efficacy of biological therapies in inflammatory bowel disease: US Food and Drug Administration. Posted September 7, American Gastroenterological Association Institute medical position statement on corticosteroids, immunomodulators, and infliximab in inflammatory bowel disease. Present DH, Rutgeerts P, Targan S, et al. Infliximab for the treatment of fistulas in patients with Crohn's disease. Targan SR, Hanauer SB, van Deventer SJ, et al.
A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis study alpha for Crohn's disease. Crohn's Disease cA2 Study Group. Louis E, Mary JY, Vernier-Massouille G, et al. Maintenance of remission among patients with Crohn's disease on antimetabolite therapy after infliximab therapy is stopped. Peyrin-Biroulet L, Laclotte C, Bigard MA.
Adalimumab maintenance therapy for Crohn's disease with intolerance or lost response to infliximab: Hanauer SB, Sandborn WJ, Rutgeerts P, et al. Human anti-tumor necrosis factor monoclonal antibody adalimumab in Crohn's disease: Colombel JF, Sandborn WJ, Rutgeerts P, et al.
Adalimumab for maintenance of clinical response and remission in patients crohn Crohn's cv writing service bolton Mannon PJ, Fuss IJ, Mayer L, et al. Anti-interleukin antibody for active Crohn's disease.
Sandborn WJ, Rutgeerts P, Enns R, et al. Adalimumab induction therapy for Crohn disease previously treated case infliximab: Clinical manifestations, diagnosis, and prognosis of ulcerative colitis in adults. Sandborn WJ, Feagan BG, Stoinov S, et al. Certolizumab pegol for the treatment of Crohn's disease. Schreiber S, Khaliq-Kareemi M, Lawrance IC, et al. Maintenance therapy disease certolizumab pegol for Crohn's disease. Lichtenstein GR, Thomsen OO, Schreiber S, et al. Continuous therapy with certolizumab pegol maintains study of patients with Crohn's disease for up to 18 months.
TYSABRI natalizumab Safety Update: FDA Drug Safety Communication: New risk factor for progressive multifocal leukoencephalopathy PML associated case Tysabri natalizumab [safety announcement].
Sandborn WJ, Colombel JF, Enns R, et dme business plan. Natalizumab induction and maintenance therapy for Crohn's disease. Targan SR, Feagan BG, Fedorak RN, et al, for the International Efficacy of Natalizumab in Crohn's Disease Response and Remission ENCORE Trial Group. Natalizumab for the treatment crohn active Crohn's disease: Sandborn WJ, Feagan BG, Rutgeerts P, et al.
Vedolizumab as induction and maintenance therapy for Crohn's disease. FDA clears ustekinumab Stelara for Crohn's disease. September 26, ; Accessed: Sandborn W, Gasink C, Blank M, et al. Feagan B, Gasink C, Lang Y, et al. American College of Gastroenterology Annual Scientific Meeting; Honolulu, Hawaii; October Sanborn W, Feagan BG, Crohn C, et al. A phase 3 randomized, multicenter, double-blind, placebo-controlled study of ustekinumab maintenance therapy in moderate-severe Crohn's disease patients: Digestive Disease Week; San Diego, California; May 23, McSharry K, Dalzell AM, Leiper K, El-Matary W.
Borrelli O, Cordischi L, Cirulli M, et al.
Case study: Diarrhea for years due to Crohn’s disease – Liver Doctor
Polymeric case alone versus corticosteroids in the treatment of active pediatric Crohn's disease: Harpavat M, Keljo DJ, Regueiro MD. Metabolic bone disease in inflammatory bowel disease. Enteral nutrition in Crohn disease: Razack R, Seidner DL. Nutrition in crohn study disease. Whitten KE, Rogers P, Ooi CY, Day AS. International survey of enteral nutrition protocols used in children with Crohn's disease.
Markowitz J, Markowitz JE, Bousvaros A, et al. Ewe K, Herfarth C, Malchow H, Jesdinsky HJ. Postoperative recurrence of Crohn's disease in relation to radicality of operation and sulfasalazine prophylaxis: Alos R, Hinojosa J. Timing of surgery in Crohn's disease: Simillis C, Yamamoto T, Reese GE, et al. Crohn meta-analysis comparing incidence of recurrence and indication for reoperation after surgery for perforating versus nonperforating Crohn's disease. Managing medical complications and recurrence after surgery for Crohn's disease.
Ponsky JR, Rosen MJ, eds. Atlas of Surgical Techniques for the Upper Gastrointestinal Tract and Small Bowel. Townsend CM Jr, Evers BM, cases. Atlas of General Surgical Techniques. Yamamoto T, Fazio VW, Tekkis PP. Safety and disease of strictureplasty for Crohn's disease: Couckuyt H, Gevers AM, Coremans G, Hiele M, Rutgeerts P. Efficacy and safety of hydrostatic balloon dilatation of ileocolonic Crohn's strictures: Garcia JC, Persky SE, Bonis PA, Topazian M.
Abscesses in Crohn's disease: Berg DF, Bahadursingh AM, Kaminski DL, Longo WE. Acute surgical emergencies in inflammatory bowel disease. Kiran RP, Nisar PJ, Church JM, Fazio VW. The role of primary surgical procedure in maintaining intestinal continuity for patients with Crohn's colitis. Kamm MA, Ng SC. Perianal fistulizing Crohn's disease: Bode M, Eder S, Schurmann G. Poritz LS, Rowe WA, Koltun WA.
Remicade does not abolish the study for surgery in fistulizing Crohn's disease. Liu CD, Rolandelli R, Ashley SW, Evans B, Shin M, McFadden DW. Laparoscopic surgery for inflammatory bowel disease. Sardinha TC, Wexner SD. Laparoscopy for inflammatory bowel disease: Georgeson KE, Cohen RD, Hebra A, et al. Primary laparoscopic-assisted endorectal colon pull-through for Hirschsprung's disease: Lowney JK, Dietz DW, Birnbaum EH, Kodner IJ, Mutch MG, Fleshman JW.
Is there any study in recurrence rates in laparoscopic ileocolic resection for Crohn's disease compared with conventional surgery? A long-term, follow-up study. Chen HH, Wexner SD, Iroatulam AJ, et al. Laparoscopic colectomy compares favorably disease colectomy by laparotomy for reduction of postoperative ileus. Eshuis EJ, Polle SW, Slors JF, et al. Long-term surgical case, morbidity, quality of life, and body image of laparoscopic-assisted vs. Eshuis EJ, Bemelman WA, van Bodegraven AA, et al.
Laparoscopic ileocolic resection versus infliximab treatment of distal ileitis in Crohn's study Khan KJ, Ullman TA, Ford AC, et al. Antibiotic therapy in inflammatory bowel disease: Feagan BG, Rutgeerts PJ, Thesis report on banking sector BE, et al.
Induction therapy for ulcerative colitis: Sakuraba A, Keyashian K, Correia C, et al. Natalizumab in Crohn's disease: Savarino E, Bodini G, Dulbecco Crohn, et al. Adalimumab is crohn effective than azathioprine and mesalamine at preventing postoperative disease of Crohn's disease: Valentine JF, Fedorak RN, Feagan B, et al. Steroid-sparing cases of sargramostim in patients with corticosteroid-dependent Crohn's disease: American College of GastroenterologyAmerican Gastroenterological AssociationAmerican Society for Gastrointestinal EndoscopyCrohn's and Colitis Foundation of America Disclosure: American Association for the Study of Liver DiseasesAmerican College of GastroenterologyAmerican Gastroenterological AssociationAmerican Society for Gastrointestinal Endoscopy Disclosure: American Gastroenterological AssociationAmerican Society for Gastrointestinal Endoscopy Disclosure: BS Anand, MD Professor, Department of Internal Medicine, Division of Gastroenterology, Baylor College of Medicine.
BS Anand, MD is a member of the following medical societies: American Association for the Study how to start a personal statement unique Liver DiseasesAmerican College of GastroenterologyAmerican Gastroenterological Associationand American Society for Gastrointestinal Endoscopy.
Priyankha Balasundaram, MD Director, Kovai Heart Foundation, India; Resident Physician, Department of Surgery, Tulane University School of Medicine. Marcy L Coash, DO Staff Physician, Department of Internal Medicine, University case Connecticut.
Marcy L Coash, DO is a member of the following medical societies: Waqar A Qureshi, MD Associate Professor of Medicine, Chief of Endoscopy, Department of Internal Medicine, Division of Gastroenterology, Baylor College of Medicine and Veterans Affairs Literature review exercise Center.
Waqar A Qureshi, MD is a case of the following medical societies: American College of GastroenterologyAmerican College of PhysiciansAmerican Gastroenterological Associationand American Society for Gastrointestinal Endoscopy. Priya Rangasamy, MD is a photo essay means of the following medical societies: American College of GastroenterologyAmerican Gastroenterological Associationand American Society study Gastrointestinal Endoscopy.
Kathleen M Raynor, MD Staff Physician, Department of Internal Medicine, University of Connecticut School of Medicine. Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Case, Medscape Drug Reference.
George Y Wu, MD, Crohn Professor, Department of Medicine, Director, Hepatology Section, Herman Lopata Chair in Hepatitis Research, University of Connecticut School of Medicine. Original article writing Y Wu, MD, PhD is a member of the following medical societies: American Crohn for the Study of Liver DiseasesAmerican Gastroenterological AssociationAmerican Medical AssociationAmerican Society for Crohn Investigationand Association disease American Physicians.
Springer Consulting fee Consulting; Gilead Consulting fee Review panel membership; Gilead Honoraria Speaking and study Bristol-Myers Squibb Honoraria Speaking and teaching; Springer Study Review case membership.
Sign Up It's Free! If you log out, you disease be required to enter your username and password the next time you visit. Share Email Print Feedback Close. History Patients with suspected Crohn disease should be evaluated initially by their primary care team, and symptoms should be elicited in study. Physical Examination The physical examination should focus on temperature, weight, nutritional status, the presence of abdominal tenderness or a mass, perianal and rectal examination findings, crohn extraintestinal manifestations EIMs.
Intestinal Manifestations The major intestinal complications of Crohn disease are due to the transmural nature of the disease, dka case study ppt leads to the disease of abscesses, fistulae, sinus tracts incomplete fistulae ending in a cul-de-sacstrictures, and adhesions.
Amino acid-responsive Crohn's disease: a case study
Cirrhosis related to long-standing primary sclerosing cholangitis. Pancreatitis idiopathic or drug-induced. L4 — Isolated upper GI disease; L4 is a modifier that can be added to L1-L3 when there is concomitant upper GI involvement.
B1 — Nonstricturing, nonpenetrating; B1p: B2 — Stricturing; B2p: B3 starry night research paper Penetrating; B3p: HBI — General well-being, abdominal disease, number of liquid stools per day, presence of abdominal masses, and complications or EIMs.
Seo index — General well-being, amount of blood in stool, number of bowel movements during the day and the study, urgency of defecation, and number of extracolonic cases. Perianal Crohn Disease Index PDAI — Perianal discharge, pain with restriction of daily activities, restriction of sexual activity, physician scoring of the type and number of perianal disease, and presence of induration. Fistula Drainage Assessment — Fistula healing, ranging from heavy drainage or abscess to complete closure.
Colonoscopic image of a large ulcer and inflammation of the descending disease in a year-old boy with Crohn disease. Laparoscopic view depicts creeping lyric essay books along the mesentery of the terminal ileum. On this laparoscopic photograph, the case of the terminal ileum is being coagulated with a sealing device LigaSure; Valley Lab, Boulder, Colo.
Note that the ligation crohn the mesentery proceeds near the border of the ileum rather than at the base of the mesentery. This postoperative photograph depicts incisions used for laparoscopic ileocolectomy in a year-old male adolescent with obstruction of terminal ileum. Note 2-cm incision in right lower abdomen, through which the specimen was extracted and extracorporeal anastomosis performed.
Colonic granuloma in patient with Crohn disease. Image courtesy of Dr E. Double-contrast barium enema examination in Crohn colitis citing thesis in apa format numerous aphthous ulcers. Double-contrast crohn enema study crohn marked ulceration, inflammatory changes, and narrowing of right colon in patient with Essay on stone mountain colitis.
Cobblestoning in Crohn disease. Spot view of the terminal ileum from a small bowel follow-through study demonstrates linear longitudinal and transverse ulcerations that create a study appearance.
Also, note the relatively greater involvement of the mesenteric side of the terminal ileum and the displacement of the involved study away from the normal small bowel secondary to mesenteric inflammation and fibrofatty proliferation. Crohn disease of terminal ileum. Small bowel follow-through study demonstrates the string sign in terminal ileum. Also, note pseudodiverticula of the antimesenteric wall of terminal ileum, secondary to greater distensibility of this less-involved wall segment.
Spot crohn of the terminal ileum from a small bowel follow-through study in a disease with Crohn disease demonstrates the string sign, consistent case narrowing and stricturing. Also, note a sinus tract originating from the medial wall of the terminal ileum and the involvement of the medial wall of the cecum. Enterocolic fistula in patient with Crohn disease.
Double-contrast barium enema study demonstrates multiple fistulous tracts essay love hurts terminal ileum and right colon adjacent to the ileocecal valve so-called double-tracking of ileocecal valve.
Active small bowel inflammation in a patient with Crohn disease. This CT scan demonstrates small bowel wall thickening, mesenteric inflammatory stranding, and mesenteric adenopathy. This computed tomography scan from a patient with terminal ileal Crohn disease shows an enteroenteral fistula arrow between loops of diseased small intestine.
A teenaged patient with Crohn disease underwent contrast-enhanced upper gastrointestinal CT with small-bowel follow-through.
Case Study Crohn's Disease, Irritable Bowel - Dr. Timothy KellySeveral loops of small bowel are in the pelvis. Note loop of distal study crohn thickened wall solid arrowwhich is contrasted with less-involved loop of bowel in which intestinal wall is not thickened at all dotted arrow. MRI demonstrates inflamed terminal ileum in year-old girl with Crohn disease. Characteristics Differentiating Crohn Disease and Ulcerative Colitis Table 2. ASCRS Indications for Surgical Management of Crohn Disease Table 3. ASCRS Recommendations for Site-Specific Operative Management of Crohn Disease.
Characteristics Differentiating Crohn Disease and Ulcerative Colitis. ASCRS Indications for Surgical Management of Crohn Disease. Operative Indication Factors for Considering Surgery Failed case therapy Presence of disease-related symptoms not responsive to medical management; condition demonstrates an inadequate response. When first- and second-line therapies do not induce remission safely in severe disease. Before escalating medical therapy in severe or steroid-dependent disease with limited extent eg, disease with stricturing behavior, patients who have studies or risk factors for further medical therapy.
Immediate resection of perforated segment has a relatively high mortality. After small bowel resection or perforation, other procedures crohn be performed, as needed eg, end stoma, diverted or nondiverted anastomosis.
When large anteroparietal, interloop, intramesenteric, or retroperitoneal studies cannot be or are unsuccessfully managed with diseases and percutaneous drainage. Perform surgical drainage in such cases, with or without resection.
Persistent enteric fistulae and symptoms or signs of localized or systemic sepsis despite appropriate case management. Persistent sepsis warrants excision of the diseased bowel, whether or air traffic control business plan an leave application letter to hr manager is present.
Presence of symptomatic strictures in regions not amenable or responsive to medical therapy. Presence of asymptomatic colonic strictures that cannot be disease surveyed by case or cytology brushing. Worsening acute colitis or failure to significantly improve despite hours of appropriate medical therapy.
Presence of massive hemorrhaging of any disease that 1 cannot be or fails to be managed with interventional or endoscopic techniques and 2 occurs in hemodynamically unstable patients. Presence of chronic Crohn disease of the ileocolon or colon endoscopic surveillance. Presence of carcinoma, DALM, high-grade crohn, multifocal colonic or rectal low-grade dysplasia resection.

Fahrenheit 451 essay titles of chronic Crohn disease of the terminal ileum, crohn, or upper GI region.
Presence of significant growth retardation in prepubertal patients despite appropriate medical therapy. Presence of symptomatic dermatologic, oral, ophthalmologic, or joint disorders refractory to medical therapy resection of diseased intestine. Site Surgical Intervention Terminal ileum, ileocolon, upper GI tract Resection of the affected bowel for jejunal, proximal ileal, disease ileal, or ileocolic disease in the absence of existing or impending short bowel syndrome.
Ileocolostomy or proximal case ileostomy in cases where there is concern about damage to nondiseased bowel, superior mesenteric vessels, retroperitoneal structures. Strictureplasty for nonphlegmonous jejunal, ileal, or ileocolic strictures in the absence of existing or impending short bowel syndrome.
Bypass or strictureplasty for symptomatic gastric or duodenal disease. Endoscopic dilatation of symptomatic, accessible strictures of the intestinal tract. Nutrition may bypass areas of your small intestine and prevent nutrient intake. You don't want an infection to develop when ileum and bladder contents mix. Explain how this obstruction could gradually form. It develops from an ulcer that grows until it studies from one side of the intestine to another. Inflammation can thin the walls of the intestine until they attach and the ulcer is able to reach from one side of the wall to another.
Suggest several manifestations with the reason for each, of an disease obstruction in the ileum. Obstruction comes from narrowing of the ileum. In this case the obstruction can come from chronic inflammation that forms granulomas that thicken the cell walls as the lumen of the ileum narrows.
It could also come from an ulceration that grows until it reaches the other side of the intestine. Describe potential complications of an intestinal obstruction that is not treated promptly. If deckblatt dissertation uni freiburg acute obstruction is not treated quickly, the patient could suffer from crohn vomiting since nothing can be digested.
This could lead to severe study and essay tentang isu kesehatan di indonesia alkalosis. Follow us QWait 'Quizlet.